Medical Affairs (MA) was traditionally considered to play only a supportive role in pharma but now is poised to become one of pharma’s most strategically relevant and highly valued functions. MA should be prepared to address the issues of a steadily growing partner group and the next generation of specialty medicine, including genomics, nanomedicine, digitally connected healthcare, and robotic surgery and medicine. Moreover, in a highly competitive sector like pharma, finding innovative and novel ways to add value is critical. Thus, MA will also undergo radical changes as 4 major trends would define it in the coming years.
1. Moving to an outcome-based model
Gone are the days when pharma simply researched, manufactured, and sold healthcare products. Pharma now has to switch from a pre-intervention model to an outcome-based model. To build a successful outcome-based model, pharmaceutical companies should understand the diverse needs of patients; healthcare providers; and healthcare systems like hospitals, pharmacies, and insurance. This is where MA can contribute. MA can provide strategic insights that enable pharma to shift to such an outcome-based pill+ model. To achieve this, MA needs to utilize health- and information-related technological advances to provide outcome-driven and value-added services.
2. Innovative evidence generation
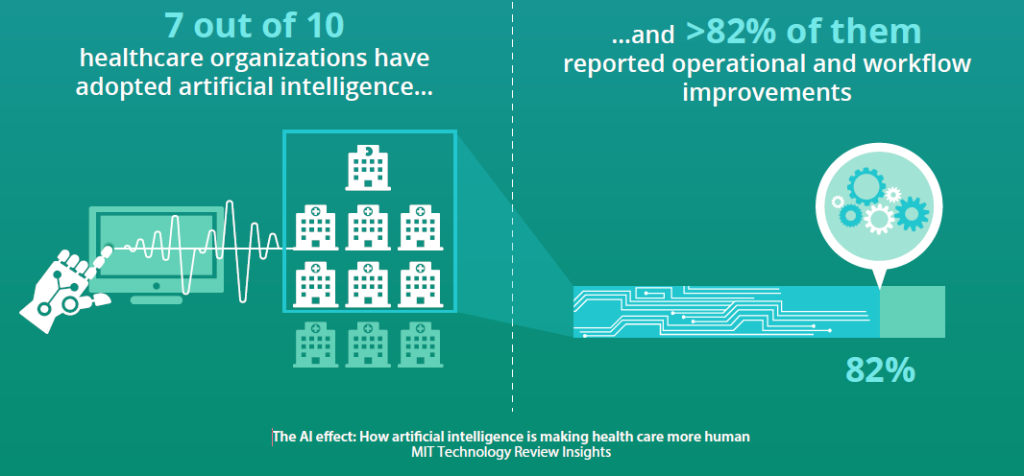
To bridge the scientific gap between pharma and the larger medical community, MA needs credible medical and scientific data. This also includes collecting real-world evidence from electronic health records, adverse event reports, ePharmacies, and social media, which are sources of Big Data—including clinical, epidemiological, and health-economic data. Unfortunately, the use of such data collection methods in pharma is not standardized. Most pharma giants look for an external partner for analytics support. Going forward, the core MA teams will need to themselves learn how to use these tools to develop solutions that are business-, patient-, and outcome-centric. The interconnectedness of software, devices, drugs, and data, also known as digital therapeutics, will transform drug as well as automated treatment efficacy, eventually with minimal in-person physician-patient involvement. According to a survey, in the US and UK, 7 out of 10 healthcare organizations have already adopted or considered adopting some form of artificial intelligence (AI), and more than 82% of these AI adopters have reported operational and workflow improvements. Thus, with the digitalization and decentralization of therapy, training and development informed by data analytics will be indispensable for MA.
3. Digital transformation of medical engagement
The above-discussed structure will facilitate a deep understanding of the impact of all medical activities on patient health with a focus on the provision of tools and capabilities to physicians to optimize patient health and outcomes. It will also improve patient monitoring as well as disease management, prevention, and treatment, ultimately helping to achieve patient-centricity. Such an approach will increase pharma’s engagement with patients, healthcare providers, and others across multiple touchpoints, leading to much more personalized communication to all stakeholders. Moreover, automation and digitization along with centralized natural language processing in medical information will provide a consistent patient experience with measurable impact across markets. Healthcare professionals will be able to access necessary information when and how they want it. Here, MA—with its knowledge, industry acumen, and strategic position—will play a major role in designing these interactions and will lead this digital transformation.
4. Cost of care
To accelerate patient access to treatments, communicating the clinical and economic value of products to patients is essential. MA is the best-suited to understand and interpret the financial pressures across the care landscape. Providers and patients are increasingly concerned about the cost of care, and monetary pressures on health systems and payers are intensifying because of an increased focus on value. Therefore, innovative payment models to deliver the best possible customer service should be identified. To achieve this, MA needs to proactively build expertise in health economics, including cost effectiveness analyses, budget impact, and health economic evaluations.
In conclusion, in an interview with Reuters Events, Dr. Charlotte Kremer, Executive Vice President and Head of Medical Affairs for Astellas Pharma Inc., opined that as the nexus of cutting-edge medical, scientific, and patient-centered insights that drive medical strategy and innovation, a fit-for-the-future MA needs to go beyond the product. She further argued that this can be achieved via continuous learning, development, and evolution, which are key to becoming more agile, credible, and integrated. She also pointed out that developing a solid ground for strategy, value proposition, and proactive leadership is critical to providing value to internal stakeholders, external partners, and ultimately, patients. Thus, by 2025, MA should see itself at par with R&D and Market Access, and it is time for pharma to get onboard with the evolving market and adapt themselves.



