Patient advocacy stands at the forefront of patient-centered care, dedicated to enhancing treatment outcomes and patient safety. While patient advocacy groups (PAGs)/patient advocacy organizations (PAOs) work toward supporting and promoting patients’ rights and interests within the healthcare system, they are also important stakeholders in formulating healthcare policies, disseminating valuable patient education, and providing patient perspectives to create patient-centered treatment plans. PAGs/PAOs have active representation in national guideline committees and potentially contribute to (either by advocating or funding) basic and clinical research in therapy areas of interest.
Patient advocacy in the biopharma landscape is being increasingly prioritized based on a reignited focus on patient-first strategies. Key focus themes include striving toward equitable access to healthcare, inclusivity of diverse patient groups in clinical trials, addressing unmet needs with an emphasis on patient perspectives, and fostering meaningful engagement between stakeholders for the benefit of patients.
However, patient advocacy engagement isn’t just about visibility and input. It’s also about effective and efficient collaboration—making the most of every touchpoint inside and outside the healthcare system to address patients’ needs in relevant, actionable ways. Below are the crucial elements that contribute to an effective approach to patient advocacy.
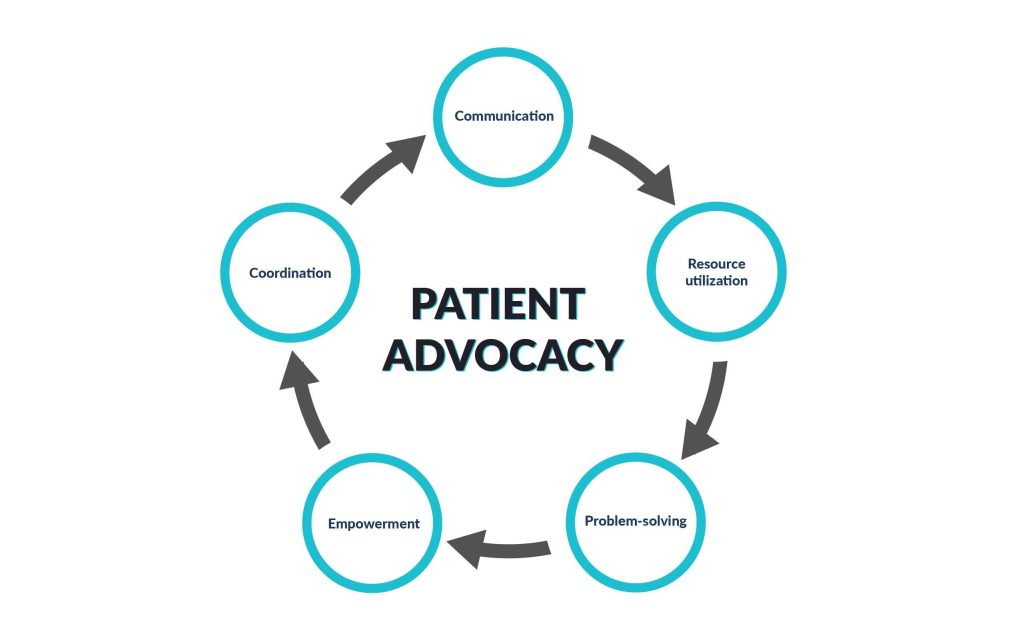
Figure 1: Key components of effective patient advocacy
- Communication: Clear and effective communication among fellow patients, caregivers, and families is paramount, and PAGs may receive support from other stakeholders (ex: biopharma) to prioritize patients’ unmet needs and preferences. PAGs build a community where patients feel accepted and act as a trusted resource, giving patients access to other patients.
- Resource utilization: Efficiently connecting patients with the resources and support services they need is a key objective for patient advocacy.
- Problem-solving: Stakeholders work to effectively overcome the barriers and challenges associated with advocating for patients’ rights.
- Empowerment: Patients are empowered through education, which encourages self-advocacy and facilitates informed decision-making.
Coordination: Effective collaboration involves seamless coordination and communication among all parties involved in patient care [healthcare providers (HCPs), social workers, insurance companies, biopharma companies, etc.] to help relieve disease burden.
End-to-end patient involvement, a major theme in patient-centric design and care, validates the importance of integrating patients across all stages of the drug development lifecycle: from input into research design through dissemination of trial results post-approval and follow-ups for safety post-marketing. Research shows that engagement with patient groups leads to improved study cycle times, decreased patient drop-out rates, improved patient satisfaction, and better health outcomes. Biopharma partnerships with PAGs also provide mutual benefits beyond clinical trials and are rapidly becoming the norm in drug development and beyond.
- Collaboration with patient groups is becoming increasingly relevant in rare diseases to garner patient perspectives and accelerate the development of targeted therapies.
- PAGs actively work toward policies and regulations connected with expedited drug approvals, access to affordable medications, transparency in drug pricing, etc. Biopharma companies that engage with these advocacy efforts demonstrate a commitment to patient welfare beyond commercial interests.
- In this era of digitalization, biopharma companies are expected to embrace digital tools for enhanced patient engagement and collaboration with PAGs/PAOs.
A view toward 2030: trends and expectations
The healthcare industry is dynamic and ever-changing, with several factors, such as technological advancements, regulatory and policy changes, and societal shifts influencing its direction. Patients have been the missing player in system-level healthcare decision-making, and PAGs have tremendous potential to change this. Based on present trajectories and emerging developments, we think that future trends in patient advocacy within the U.S. biopharma industry by 2030 could include
- Greater integration of patient input in drug development: By 2030, there will be a greater emphasis on incorporating patient perspectives and preferences into all stages of the drug development lifecycle, from early research to clinical trials and post-marketing surveillance. Biopharma companies may collaborate more closely with patients and PAGs to ensure that therapies are aligned with patient needs and priorities. Patients would no longer be viewed just as study subjects but would be sought after as protocol, methodology, and policy co-designers. Patient advocates often have firsthand experience of a medical condition, and this helps them bring patient needs and desired outcomes to the forefront, thereby challenging any associated assumptions made by biopharma or policymakers. A first-of-its-kind external guidance drafted by the Duchenne Muscular Dystrophy (DMD) community–led by Parent Project Muscular Dystrophy–serves as an example. The coalition, formed by parents of children suffering from DMD, worked across time zones to draft the guidance in a record time of six months and submitted it to the U.S. FDA, challenging the 2013 European Medicines Agency draft guidelines on muscular dystrophy drug development and approval. Such an undertaking by PAGs could be a norm by 2030.
- Heightened involvement of the FDA in patient engagement: The FDA’s relationship with PAGs and patient organizations dates back to the HIV/AIDS advocacy movement of the 1980s and 1990s. This has evolved to include a portfolio of institutional mechanisms to facilitate the patient engagement process. Further advancements incorporating patient perspectives into regulatory decision-making and policy developments are in place. Toward a more futuristic approach, patient advocacy aims to integrate a new central portfolio, Patient Affairs Staff (PAS), to support patients and their advocates in understanding the regulatory processes and navigating the FDA.
- Policy advocacy for patient-centered healthcare: Patient advocacy organizations will be prominent voices in shaping healthcare policies and regulations at both the state and federal levels. This could involve advocating for reforms that prioritize patient-centered care, improve healthcare affordability and accessibility, and strengthen patient rights and protections.
- Involvement of patients as authors: Biopharma companies, along with medical communication professionals, support the use of patient-first and patient-friendly language in publications. Further, enhancing the readability and accessibility of publications for patient communities by including plain language summaries (PLS) of publications is already being enforced. To capture valid patient perspectives and generate patient-friendly reading material, PAGs are focused on involving patients as authors. We project that PAGs will partner with biopharma and journals to develop more robust guidelines for engaging patient authors moving forward. However, the accessibility of this material to the patient community is a facet that has the potential and the need to improve in the next few years.
- Expansion of patient access programs: Biopharma companies dedicated to patient-centric care could expand their patient access programs to provide more financial assistance, support services, and educational resources to patients, especially for complex or high-cost therapies. These programs may be tailored to address the specific needs of diverse patient populations and ensure equitable access to treatments.
- Advocacy for health equity and inclusion: Patient advocacy will increase focus on addressing health disparities and promoting inclusivity within the healthcare system. This could involve advocating for policies and initiatives that improve access to healthcare services, reduce barriers to treatment, and prioritize the needs of underserved communities.
- Digital innovation in patient engagement: The use of digital health technologies for patient engagement and empowerment is likely to continue evolving. By 2030, PAGs and biopharma companies may leverage advanced digital tools, such as artificial intelligence, telemedicine, and wearable devices, to enhance patient support, facilitate communication, and collect real-time data on patient experiences. Trends related to obtaining faster real-time data to inform real-world evidence (RWE) gathering and examining will empower both patients and HCPs to make better decisions and identify what’s not working, enabling them to adapt rapidly. Moreover, companies that are currently not including patients in time for clinical trials will also have to ramp up their patient inclusion efforts quickly.
- Collaborative partnerships and advocacy coalitions: We expect increased collaboration among PAGs, HCPs, biopharma companies, and government agencies to address common challenges and advance shared goals. Advocacy coalitions focused on specific disease areas or healthcare issues may emerge to amplify collective voices and drive systemic change.
- Empowerment of patient advocates: By 2030, patient advocates will receive greater recognition as key stakeholders in the healthcare ecosystem. Patient advocacy training programs, certification pathways, and professional networks may be established to empower advocates with the skills, knowledge, and resources needed to effectively represent patient interests and drive positive change.
Overall, we predict that by 2030, the relationship between patient advocacy and U.S. biopharma is likely to be characterized by a growing emphasis on patient-centered approaches, collaborative partnerships, digital innovation, and advocacy for health equity and inclusivity.
How can biopharma be ready to strengthen patient advocacy in the future?
Despite the “greater good” approach favored by most PAGs/PAOs, there is a concern about the relationship between these organizations and the biopharma and medical device companies that provide their commercial funding. This connection has the potential to compromise the message being sent out by the PAG, making it appear like a promotional activity. To avoid the appearance of conflicts of interest, it is essential for patient organizations to work toward financial independence from industry funders and for companies to strictly adhere to their organization’s compliance rules.
In this context, Medical Affairs is uniquely positioned to act as a vital bridge, connecting the biopharma industry with the lay public and addressing the mistrust that often exists. By leveraging their in-depth knowledge of the healthcare landscape and commitment to patient-centric care, Medical Affairs can help ensure that the collaboration between biopharma and patient advocacy groups remains transparent and aligned with genuine patient interests. This role is not only crucial in dispelling doubts about the motivations behind patient advocacy but also in reinforcing the credibility of PAGs as independent voices for patient welfare.
As we look toward 2030, the evolving landscape of patient advocacy within the biopharma industry will increasingly rely on the leadership of Medical Affairs. Their role in fostering trust and collaboration between stakeholders will be pivotal in advancing patient-centered care. By integrating patients into more facets of their business and by focusing on transparency, independence, and alignment with patient interests, Medical Affairs can help drive a stronger push for patient-centric care. Those who heed this call today are positioned to be the leaders of tomorrow, guiding the industry toward a future where patient advocacy is more integrated, credible, and impactful than ever before.

Dr. Swapna Ganduri (PhD)
Manager, Quality and Training

